Wolfe did a great job, and did REAL verifiable experimentations, ones ANYONE can do. His article is HERE.
Great article Wolfe, dovetails with my research and real world, I am reposting my link on hypercapnia under yours. The cumulative affects of BOTH too little O2 (Oxygen) and too MUCH CO2 (carbon dioxide) are going to be DEVESTATING. The O2 has the cognitive effect you mentions, but couple that with the CO2 displacement in place of the depleted O2 and you literally have acidic blood going to major organs.
We are being LIED to. WE ALL KNOW what to do, we always HAVE. What is the FIRST thing recommended in a carbon MONoxide poisoning? Remove to FRESH air, in severe cases PURE Oxygen is applied.
If it WORKS for CO, it WORKS for CO2. IF MORE Oxygen and fresh air is the curative for CO it is the curative for CO2. IF LESS Oxygen is BAD, how can a mask which you PROVED creates a lower Oxygen level be GOOD.
IF CO in place of Oxygen is BAD, so is O@, and if we are FORCED by masks to decrease the inflow of O@ while simultaneously DEGREASING the outflow of CO2.
BASIC health class, BASIC Biology.
Humans BREATHE IN Oxygen, the lungs oxygenate the blood, and Carbon DIXODE IE WASTE is exhaled.
There is a LEVEL of Oxygen REQUIRED in an atmosphere, or we will QUICKLY pass out and DIE. It is called a confined space protocol. Ever see those plastic yellow hoses going into a manhole?
They are NOT removing bad air, they are supplying FRESH air to a low oxygen area.
The hazards associated confined spaces include:
Toxic Atmosphere. A toxic atmosphere may cause various acute effects, including
impairment of judgement,
unconsciousness and death. …
Oxygen Deficiency. …
Oxygen Enrichment. …
Flammable or Explosive Atmospheres. …
Flowing Liquid or Free Flowing Solids. …
Excessive Heat.
Based on OSHA guidelines, a confined space is considered to have safe oxygen levels if readings are between 20.8-21 percent, while a space with readings of less than 19.5 percent are considered to be oxygen deficient.
Now put ALL you said, and couple that with this article https://politicalprognosticator.politics.blog/2020/08/10/your-mask-is-not-protecting-you-in-fact-it-is-most-likely-making-you-sick
and then combine that with the health and biology classes we ALL had around 4th grade, and THINK.
Masks CREATE a verifiable LOW oxygen intake.
Masks create a verifiable HIGH CO2 intake and a LOW CO2 outflow.
CO2 is HEAVIER than Oxygen, and it WILL replace it in the bloodstream. THAT makes it CUMULATIVE.
Gee THIS sounds BAD
(ăs-fĭk′sē-ə) A condition in which an extreme decrease in the concentration of oxygen in the body accompanied by an increase in the concentration of carbon dioxide leads to loss of consciousness or death. Asphyxia can be induced by choking, drowning, electric shock, injury, or the inhalation of toxic gases.
How about THIS
Although they can vary from person to person, the most common hypoxia symptoms are:
Changes in the color of your skin, ranging from blue to cherry red.
Confusion.
Cough.
Fast heart rate.
Rapid breathing.
Shortness of breath.
Slow heart rate.
Sweating.
Or THIS
Cerebral hypoxia
Email this page to a friend Print Facebook Twitter Pinterest
Cerebral hypoxia occurs when there is not enough oxygen getting to the brain. The brain needs a constant supply of oxygen and nutrients to function.
Cerebral hypoxia affects the largest parts of the brain, called the cerebral hemispheres. However, the term is often used to refer to a lack of oxygen supply to the entire brain.
Causes
In cerebral hypoxia, sometimes only the oxygen supply is interrupted. This can be caused by:
Breathing in smoke (smoke inhalation), such as during a fire
Carbon monoxide poisoning
Choking
Diseases that prevent movement (paralysis) of the breathing muscles, such as amyotrophic lateral sclerosis (ALS)
High altitudes (GEE LIKE FLYING IN AN AIRPLANE WITH A MASK ON, OR being in DENVER with a MASK ON)
Pressure on (compression) the windpipe (trachea)
Strangulation
ALL those and still we have THIS
Hypoxia[1] is a condition in which the body or a region of the body is deprived of adequate oxygen supply at the tissue level. Hypoxia may be classified as either generalized, affecting the whole body, or local, affecting a region of the body.[2] Although hypoxia is often a pathological condition, variations in arterial oxygen concentrations can be part of the normal physiology, for example, during hypoventilation training or strenuous physical exercise.
Hypoxia differs from hypoxemia and anoxemia in that hypoxia refers to a state in which oxygen supply is insufficient, whereas hypoxemia and anoxemia refer specifically to states that have low or zero arterial oxygen supply.[3] Hypoxia in which there is complete deprivation of oxygen supply is referred to as anoxia.
Generalized hypoxia occurs in healthy people when they ascend to high altitude, where it causes altitude sickness leading to potentially fatal complications: high altitude pulmonary edema (HAPE) and high altitude cerebral edema (HACE).[4] Hypoxia also occurs in healthy individuals when breathing mixtures of gases with a low oxygen content, e.g. while diving underwater especially when using closed-circuit rebreather systems that control the amount of oxygen in the supplied air.
and then finally
Hypercapnia (from the Greek hyper = “above” or “too much” and kapnos = “smoke”), also known as hypercarbia and CO2 retention, is a condition of abnormally elevated carbon dioxide (CO2) levels in the blood. Carbon dioxide is a gaseous product of the body’s metabolism and is normally expelled through the lungs.
What are symptoms of high co2 levels?
Symptoms
dizziness.
drowsiness.
excessive fatigue.
headaches.
feeling disoriented.
flushing of the skin.
shortness of breath.
Over time, the MORE CO2 you take in in PLACE of Oxygen (because of the mask restriction) BUILDS UP. It does NOT go away rapidly, and once it reaches a certain level, BAD things happen. It CHANGES your blood PH, making it ACIDIC, and THAT destroys the ORGANS first. Thinks like the Heart, Liver, Kidneys, Lungs, and BRAIN.
The mask LIE is making you listless, sick, and COULD be killing you in secret by attacking other organs especially the kidneys. The point is you WON’T really know until it is BAD, and perhaps too late.
Masks are made for SHORT term use, ACUTE exposures, not everyday consistent use.
Why no medical professional does what Wolfe and I have done, and puts it to clinical STUDY is beyond me.
TWO more things, underlying health problems like COPD, Hypertension, Heart problems, and SMOKING make it ALL worse.
We will NOT know the TRUE effects or COSTS of mask use for YEARS. THAT is the insidious part, lasting chronic effects coming.
An OLD colleague once said. Sometimes, the CURE is WORSE than the DISEASE.
THAT is masks in a nutshell.
Thank you for this excellent post. Very important info and easy for everyone to comprehend and relate to. I am passing it on to friends.
LikeLiked by 2 people
Please do! people need to know the TRUTH.
LikeLiked by 1 person
My brother’s family has so bought the masks help hype! We will share this to see if it will help.
LikeLiked by 1 person
P-Rex said: “CO2 is HEAVIER than Oxygen, and it WILL replace it in the bloodstream. “
…
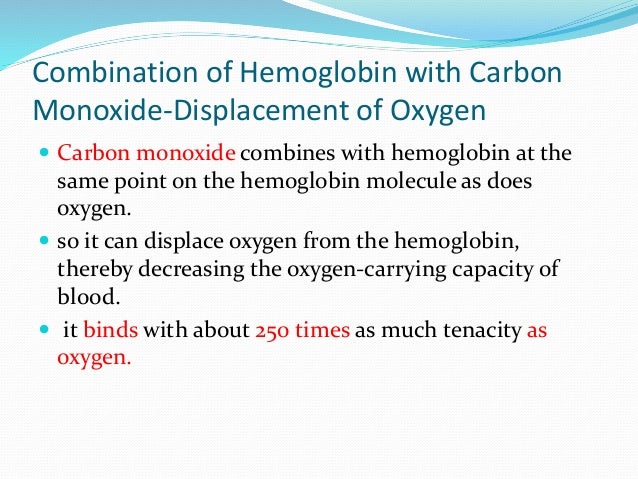
No, this is incorrect. Heavier has nothing to do with it. It is Hemoglobin’s Affinity for CO or CO2 or O2.
Hemoglobin has to GRAB O2 BUT NOT SO HARD that it does not release it to the cells. With CO, the affinity is so high CARBON MONOXIDE STAYS BONDED TO HEMOGLOBIN AND WILL NOT LET GO UNTIL the O@ partial Pressure is VERY HIGH! <=== Critical point and applies to CO2 also.
(P = partial pressure aka the amount of gas in a volume of gas at a set pressure.)
(Slide 54)
There are two good slide show on O2 and CO2 in the lungs and blood. (Note how they CAREFULLY avoid the topic of CO2 and O2 in the atmosphere you are breathing.)
Hemoglobin dissociation equilibrium constants O2, CO2
Transport of oxygen and carbon dioxide in blood (A for this slide show)
*https://www.slideshare.net/LubnaAbuAlRub/transport-of-oxygen-and-carbon-dioxide-in-blood-1
A second Slide show gas exchange in the lungs: (B for this slide show)
*https://www.slideshare.net/maswazi10/unit-3-respiratory-system-and-gas-exchange?next_slideshow=1
Slides A 27, 28 & A-31 are the critical slides:
One slide (A-30) show mentions “Alveolar Carbon Dioxide” So I went hunting:
https://image.slidesharecdn.com/transportofoxygenandcarbondioxideinblood1-150803065608-lva1-app6891/95/transport-of-oxygen-and-carbon-dioxide-in-blood-1-30-638.jpg?cb=1438585276
Alveolar Carbon Dioxide
Qualitatively, the partial pressure of carbon dioxide within the alveoli is determined by two opposing processes. The first involves entry of carbon dioxide into the alveolus and occurs due to diffusion of carbon dioxide gas from the pulmonary capillaries into the alveolar space (This process is discussed in Carbon Dioxide Pulmonary Gas Exchange). The second involves the rate at which carbon dioxide is expelled from the alveolus during refreshing of alveolar air with external air and is determined by the rate of alveolar ventilation. The balance between these two opposing processes ultimately determines the steady-state carbon dioxide gas tension within the alveolus and can be quantitatively described using the equation below…..
.
.
.
.
• Because of the near equivalence of arterial and alveolar partial pressure of carbon dioxide, the equation above is typically unnecessary in calculating the PACO2 since the PaCO2 can be easily and directly measured by obtaining arterial blood gases. In fact, direct measurement of arterial carbon dioxide tension is typically used to calculate the alveolar ventilation rate, rather than the converse. However, we provided the extensive discussion above to demonstrate how PACO2 is dependent on the body’s metabolic production of CO2 and the alveolar ventilation rate. These considerations will become important in our discussion of alveolar oxygen in the next section.”
*http://pathwaymedicine.org/alveolar-carbon-dioxide
>>>>>>>>>>
Alveolar Oxygen
“Qualitatively, the partial pressure of oxygen within the alveoli is determined by two opposing processes. The first involves entry of oxygen into the alveolus from the external environment and is determined by the rate of alveolar ventilation as well as the starting partial pressure of oxygen in the external environment. The second involves the rate at which oxygen diffuses into the pulmonary capillaries and is carried away, a process discussed in Oxygen Pulmonary Gas Exchange. The balance between these two processes, which bring oxygen into the alveolus and then carry it away, ultimately determines the steady-state value of alveolar oxygen partial pressure.
• Quantitatively, the partial pressure of alveolar oxygen can be calculated using the “Alveolar Gas Equation” given below. The alveolar oxygen tension is of significant physiological importance as it largely determines the partial pressure of arterial oxygen. This is because the partial pressure of oxygen in the alveoli largely equilibrates with that in capillary blood by the end of the pulmonary capillaries, as discussed in Oxygen Pulmonary Gas Exchange. Consequently, derangements of the alveolar oxygen tension can and will lead to significant derangements in the arterial oxygen tension.
Overview
◦ Although the derivation for the Alveolar Gas Equation is complex and not discussed here, below we provide a largely informal qualitative explanation for the structure of the equation. Given our discussion above it may be initially unclear why terms for alveolar ventilation and the rate of oxygen diffusion into the pulmonary capillaries are not included in the equation. The student can think of these variables as subsumed under the term for alveolar carbon dioxide as discussed further below.
• Alveolar Gas Equation
◦ PAO2 = PIO2 – PACO2/R
◦ Where:
◦ PAO2 = Partial pressure of alveolar oxygen
◦ PIO2 = Partial pressure of inspired air
◦ PACO2 = Partial pressure of Alveolar Carbon Dioxide
◦ R = Respiratory Exchange Ratio
.
.
.
.
Respiratory Exchange Ratio
◦ One issue with the discussion of metabolism above is that the quantitative metabolic production of CO2 by the body is often not numerically equivalent to the metabolic production of O2. Because the value of alveolar carbon dioxide is calculated using the the rate of CO2 production, this may lead to errors when the PACO2 is used to a proxy variable for the metabolic consumption of O2 in calculating the alveolar oxygen tension. The Respiratory Exchange Ratio (R) included in the alveolar gas equation is a variable which corrects for this issue. The respiratory exchange ratio can vary and is dependent on the primary nutrients that the body is metabolizing.
◦ For example, when the body primarily metabolizes carbohydrates, the respiratory exchange ratio is approximately 1.0; however, when fats are primarily utilized, the value drops to 0.7. The dependence of the ratio on the nutrients metabolized has to do with the number of oxygen molecules required to fully metabolize the nutrient to carbon dioxide. Because carbohydrates inherently possess a large number of oxygen molecules, roughly one molecule of oxygen is required to produce one molecule of carbon dioxide; in contrast, because fats possess nearly no oxygen molecules, each molecule of oxygen produces only 0.7 molecules of carbon dioxide. In a healthy individual on an average diet, the respiratory exchage ratio is roughly 0.8….”
*http://pathwaymedicine.org/alveolar-oxygen
Sounds like kids eating high carb –Soda and candy and grain — diets are even worse off.
LikeLiked by 1 person
I have a comment in Da Bin with a couple of interesting slides.
LikeLiked by 1 person
Ok, sorry, started new job today, ill fix it. TY!
LikeLike
Congratulations on the new job!
LikeLiked by 1 person
TY, we’ll see how it goes. So far 50/50.
LikeLike